Doctors are urging Coloradans to check on their vaccination status for the measles and to consult their physician if they’re unsure of their immunity to the virus. This year, for the first time since 1996, three people in the state have tested positive for measles.
The cases come amid outbreaks in Texas and nearby states of New Mexico, Oklahoma and Kansas as well as in pockets of Indiana, Pennsylvania and Ohio. Colorado’s cases aren’t considered an outbreak since the public health definition for an outbreak is three or more related cases, and there’s no evidence that Colorado’s are linked.
We reached out to Dr. Clint Sowards, a family physician with San Luis Valley Health in Antonito to get his take on measles cases in Colorado and ask what he’s recommending to patients.
This transcript has been edited for content and clarity
Many doctors practicing in the U.S. have never seen a case of measles. As a physician, have you ever seen a case of measles?
“No. I am one of those that have never seen a case!”
Is there less reason for concern about the spread of measles in Colorado since the cases aren’t linked?
“I wouldn't say less concern. I think any amount of cases in your region or state should be concerning, especially in a largely vaccine-preventable illness. Of course, when you have a higher frequency of illnesses and more cases pop up, the concerns should definitely rise, especially in those regions that are largely unvaccinated.”
Why are some people reluctant to get the measles vaccine?
“It comes from a couple different places. One, just a general lack of understanding of how the vaccine works and the safety and efficacy of it. But then also people remember their family, brothers and sisters getting sick with the measles and they did just fine. And … by and large, most people do just fine.”
“[But] about three out of 10 kids who get measles will experience complications. One out of 20 will end up with pneumonia. Three in a thousand may die and one in a thousand will get a swelling of their brain and spinal cord, which can be quite severe and lead to developmental delays. It's those one in a thousand, it's the ones that are high risk that we would love to prevent, especially when the vaccine is much more safe, much more efficacious, and very low risk. It is definitely safer than getting the measles itself.”
How contagious is measles compared to COVID?
“Measles is much more contagious. If you are in the same room with someone coughing, some studies suggest above 90 percent that you will get exposed to the measles. Now the difference is, did you have your vaccination? Are you prepared? Is your body prepared to fight that infection off? If not, it's highly likely you're going to fall ill with the measles. Why risk falling ill and risk a complication when you can protect yourself?”
Are you on the lookout now for measles in your area?
“Yes, [one of the cases is in] our neighboring county to the west. Of course, we at San Luis Valley Health are on high alert. We have implemented procedures to increase screenings at the door to prevent any unwanted or potential exposures that could happen if someone walks into our clinics not understanding that they potentially have the measles and could accidentally expose a lot of people to the virus.”
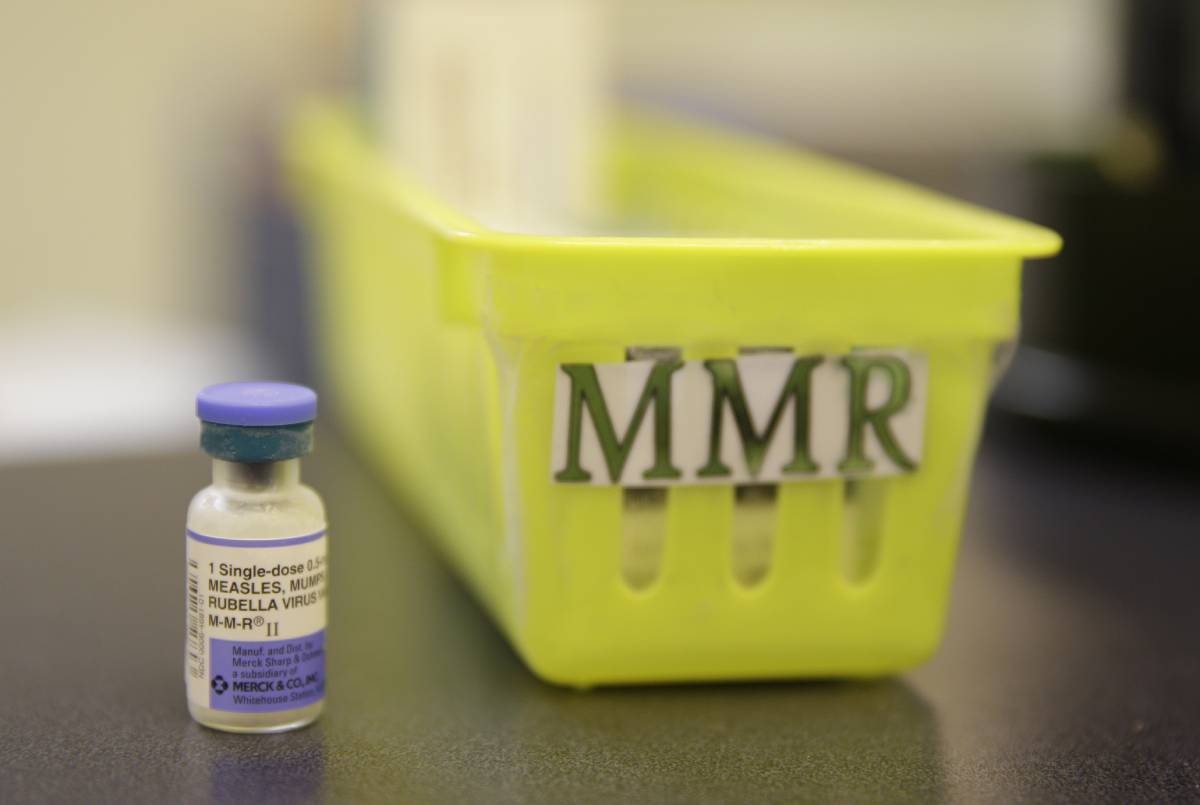
What is the risk of the MMR vaccine and how much of a chance is there that there will be side effects?
“There is a small chance that you can develop measles from the vaccine. It is a live virus, but most of the time we develop minor side effects, maybe pain and redness at the injection site, maybe feeling a little achy, maybe run a low-grade temperature that usually subsides in 24 hours.”
Have you seen any change in vaccine hesitancy recently?
“There's definitely been a change in vaccine hesitancy, I would say since the COVID vaccine. It hasn't been dramatic and maybe it's just been more obvious to me as I counsel parents and families regarding necessary vaccines. I use the example of a pendulum. We see this shift of, okay, we're doing really well. There's less vaccination numbers, they kind of drop a little bit. But then something like this happens where we have an increase in cases and we see the pendulum swing the other way, where people are more vigilant, they do get more vaccinated, they educate themselves more, and then things calm down, things are going well, and it swings back.”
Babies are unprotected from measles early on because they don't get their first measles shot until 12 to 15 months. What's your recommendation for parents with babies in terms of taking their child out, traveling?
“We are following routine scheduling at 12 months and then at four years before kindergarten. Now, in some situations, if a family is having a high frequency of international travel where they're traveling to more prevalent areas, those guidelines can shift. And the CDC has outlined specific guidelines for those families.”
“And now, a lot of [adults] don't remember their vaccination status. We think, ‘Did I get the vaccine? Was I exposed?’ If you were born before 1957, we can assume you likely had contact with it and have some immunity to the measles virus. After that, we need to dig a little deeper. Do you have documented vaccine evidence? Do you have documented immunity with specific blood tests that check your response? I know for me and my patient population, those who are at low risk [for side effects] who have no document of vaccination or immunization, I'm following the guidelines of revaccinating at least one time for that specific adult population.”









