
On Colorado's Eastern Plains, south of Interstate 70, about 100 miles southeast of Denver, is the town of Hugo, established by ranchers, later a railway town.
Lincoln Community Hospital and Care Center is here, caring for people who get in crashes on the freeway, plus a population of less than 10,000 people in an area the size of the state of Connecticut.
“Honestly, there's more cattle than there are people,” said CEO Kevin Stansbury as he greets visitors.
It was a busy day on Tuesday at the 15-bed critical access facility.
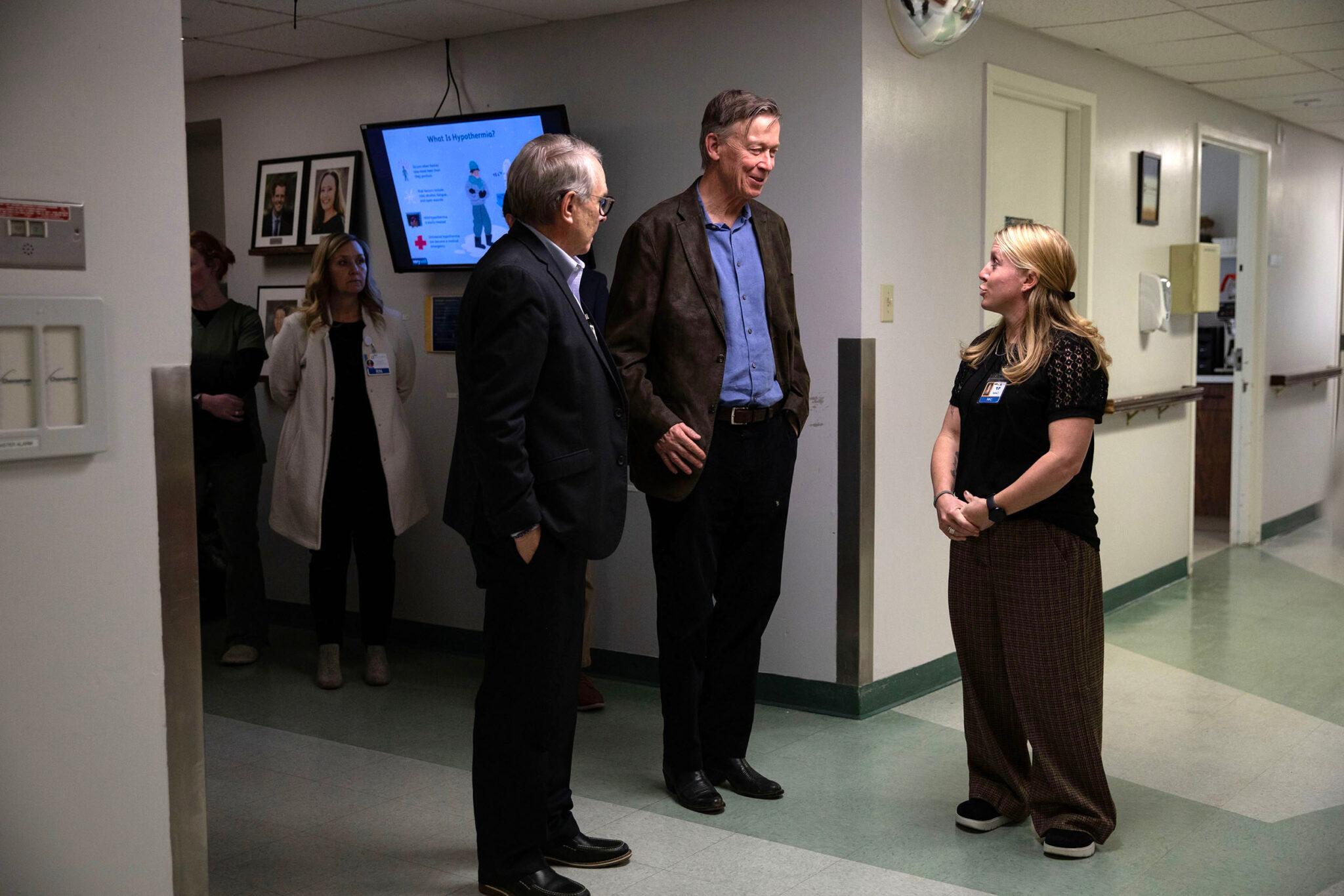
Stansbury and some other rural hospital executives hosted Sen. John Hickenlooper on a tour, looking to spotlight new storm clouds on the rural health horizon.
As they headed off down the hall, I spoke with Dr. Brianna Fox, the chief of staff at the hospital, which is the only one within a 75-mile radius of Hugo and serves Lincoln County, plus parts of Washington, Kit Carson, Elbert and Cheyenne counties.
Does she worry about the future of this facility? “Always. I really do,” said Fox.

Fox, in blue scrubs, said a shadow had been cast by nearly a trillion dollars in federal cuts to Medicaid, as part of H.R. 1, also called the One Big Beautiful Bill, and Affordable Care Act tax subsidies not getting renewed.
“The funding cuts that just came out of Washington, they slashed it huge for Colorado and how are we gonna make that up at the state level?” Fox asked.
Beyond the cuts, labor costs are going up, but government payments, reimbursements, don't cover costs for care, she explained. For example, Medicaid, which covers a lot of rural Coloradans, covers only 79 cents per dollar of care.
Around the country, more rural hospitals are failing, she warned. “We're pretty resilient, but to a finite point. And we're to the point where we're starting to drown,” Fox said, adding that the hospital was built in 1959 and needs constant maintenance. “I always joke that this place is held together with duct tape and prayers.”
The situation is pushing hospitals in more remote parts of the state to the brink, Stansbury said.
“Fifty percent of the rural hospitals in the state of Colorado right now are operating at a loss — losing more money than they're making. 70 percent are operating at a margin that is not sustainable,” he said. “I'm thrilled when my CFO tells me we have 40 days cash on hand because, ‘Yahoo!’ most of the time we operate around 30 days cash on hand.”

Labor costs are up by 39 percent, and supply costs are up by 50 percent, both figures outpacing inflation, he said. An analysis from the Shep Center at the University of North Carolina found up to 20 percent of rural hospitals, or about 300, in the U.S. face the risk of closure in the coming years.
Stansbury understands that for years, there have been warnings about rural hospitals in Colorado potentially closing due to financial headwinds. They’ve stayed open, while around the country, others have shut their doors.
“We may be the victims of our own success, and the success measured by we've been able to scratch and claw and stay open,” he said. “I think if people understood the true financial distress of most of the rural hospitals in the state, there would be much more concern.”
While Hickenlooper was visiting, Stansbury took him to visit a hill covered in dry grass to the west of the hospital. That’s the potential site of a new 92,000 square foot facility that would have clinics, surgery rooms, radiology, plus more hospital rooms, which would all be compliant with the Americans with Disabilities Act.
Total price tag: $115 million. “That's gonna be a stretch,” Stansbury said. “We can't qualify financially for that.”
He said he was trying to get legislation introduced in Congress that would change the way USDA, the U.S. Department of Agriculture, surprisingly, the relevant federal agency, finances new rural hospital construction.

The impact of rising health coverage costs
Federal changes, made since the start of the Trump administration, could mean more people are uninsured, or have bare bones plans, which cover preventive care but not comprehensive care like hospitalizations or major illness.
Janet Marschner, a contractor who does CPA work at the hospital and splits her time between Colorado and Wyoming, lost the enhanced tax credit for ACA coverage. That’s like tens of thousands of Coloradans and millions of Americans, who no longer got the credit when Congress failed to renew the subsidies for people to afford to buy insurance.
She saw her monthly premium costs double to $4,000 a month and decided to get a cheaper plan for her and her husband, a retired refinery worker.
“It feels risky to me,” she said. “I guess I'm willing to take that risk and save.”

She said she has what’s called short-term health insurance, which does not cover preexisting conditions and has other strict rules and payment caps.
Marshner said she’s had very good health insurance her whole life. Then there was a year where she and her husband were transitioning between jobs and had to go into the marketplace for coverage.
“We paid in $28,000 for health insurance for two healthy individuals. And we had over $15,000 of out-of-pocket payments,” Marschner said. “And you tell me how most Americans can afford that, and that is the marketplace.”
If people like Marschner have health issues that are not covered, hospitals like Lincoln will often still care for them, which will also drive up its uncompensated costs.
‘People will not survive if the hospitals are not there.’
Later, during a roundtable discussion, hospital executives talked with Hickenlooper about a new $50 billion rural transformation fund passed by Congress. Colorado will get $200 million a year for five years.
They told the senator the money could help. But it won't make up for what's been lost to other federal cuts.
It’s something Hickenlooper said he, too, is worried about, noting the federal law cut hundreds of millions of dollars in healthcare to pay for tax cuts for the wealthy.
“It's serious harm to these rural clinics and hospitals. And it's hard to figure out how they're going to stay in business,” he said.
Michael Hassell, CEO of Melissa Memorial Hospital, a 15-bed critical access hospital in Holyoke near the Nebraska line, said he thinks rural hospitals can still hold on.
“Are we gonna thrive under these conditions?” Hassell asked, noting he especially worries about coming cuts for the poorest Coloradans, those covered by Medicaid. “How much can the poorest among us afford the constant cuts? Why does all the money always got to come from them?”
Hassell said the full impacts of that question will become more clear in the coming months.

Other hospital executives bristled at money made available, both from the federal and state government, which also includes a major administrative burden, and lots of hoops to jump through to get the funding.
“I fully appreciate people who are leaning in and trying to provide resources to rural hospitals, but they're trying to slam a square peg into a round hole,” said Brian Bogel, CEO of Kit Carson Memorial Hospital in Burlington, a Trauma Level IV facility near the Kansas border. “Our needs are not the same. Our programs are not the same. Our physical plans are not the same. Our medical staffs are not the same.”
The CEO of another facility, Claressa Millsap, CEO of 25-bed Keefe Memorial Hospital in Cheyenne Wells, near Kansas, agreed.
“We didn't get here overnight. Every hospital is a little different,” she said. “Being able to choose how the funds are used based on what your hospital needs are, so that you can prosper, I think, is the key.”

All three said they thought rural Colorado hospitals will survive, but that the threats to the facilities and the people they serve are real.
When Coloradans, or out-of-state visitors, get sick or injured in remote parts of the state, a hospital makes all the difference.
“Cardiology and vascular, heart attacks, time is muscle. Strokes, time matters,” Millsap said. “The traumas that we all see in rural hospitals are real. People will not survive if the hospitals are not there.”
| This story is part of a collection tracking the impacts of President Donald Trump’s second administration on the lives of everyday Coloradans. Since taking office, Trump has overhauled nearly every aspect of the federal government; journalists from CPR News, KRCC and Denverite are staying on top of what that means for you. Read more here. |









