
When one Colorado mom learned of problems with overbilling by the state’s Medicaid agency that cost the state tens of millions of dollars, she was dismayed.
“It makes me really angry that they're going for the most vulnerable population without auditing themselves first,” said Ciara Stewart, a mother in Aurora and advocate for children with disabilities.
Members of the state Joint Budget Committee heard from staff this week about the extent of the overpayments, which come as they cope with a nearly $1 billion budget deficit. It will include weighing deep cuts to Medicaid that threaten funding for programs supporting thousands of Colorado families.
The state’s Medicaid program mistakenly paid contracted providers, which transport patients who use larger wheelchairs, several times more than was required. The Denver Post first reported the discrepancy. The correction is projected to save the state almost $33 million through the end of this fiscal year and $60.4 million next fiscal year, including state and federal funding.
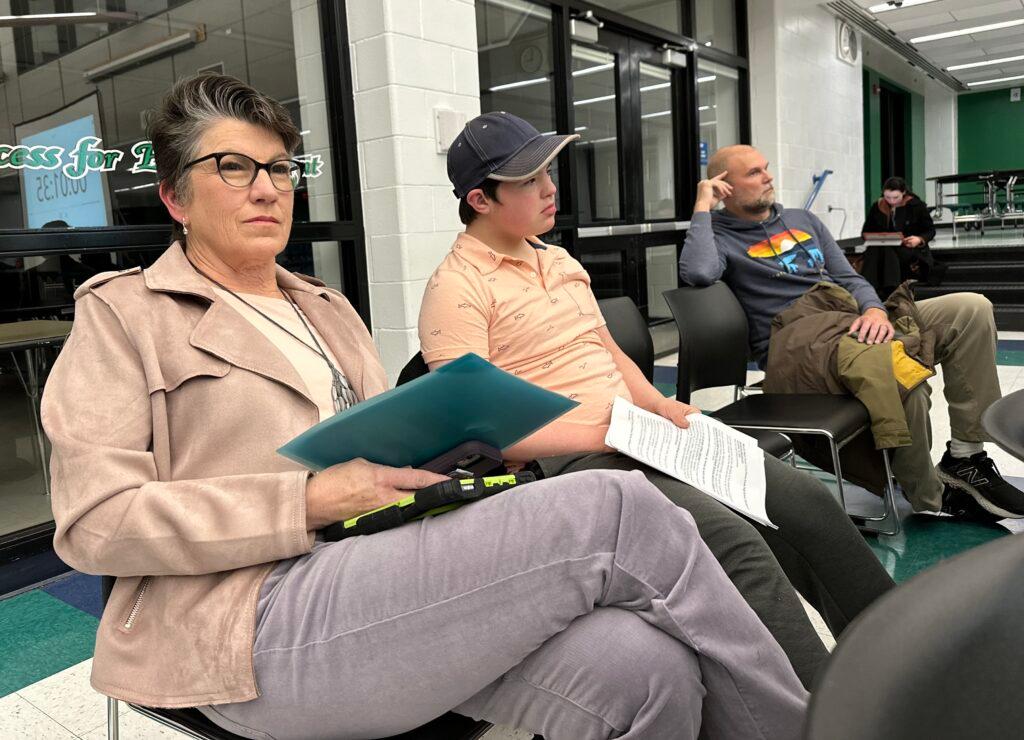
Stewart spoke to CPR before picking up her 4-year-old son, Jackson, at his school, the Anchor Center for Blind Children, in Denver.
Jackson has two rare genetic mutations, is nonverbal and non-ambulatory, and faces numerous complex developmental and medical challenges. The state's Medicaid program pays for some of the services that are crucial for Jackson.
“If the state focused on systematic billing and oversight issues, they could save significant money without harming vulnerable children and adults,” Stewart said.
She called the news heartbreaking.
“For the longest time, the narrative has felt like Medicaid costs were rising because families like mine were overusing services,” she said. “But when stories come out like this, billing errors and oversight failures, it's hard not to question that narrative. And I don't understand how something like that can happen for so long without being caught.”
Stewart estimates her son gets more than $50,000 a year in state support from a couple of programs. One is the Community Connector program that she said allows Jackson to build critical social, emotional, and communication skills in real-world environments. Taking that away during his formative years cuts off developmental opportunities that shape his future independence and well-being, she said.
In addition, Stewart said she is paid by the state to care for her son at home. But potential reductions to homemaker hours and a proposed 56-hour weekly caregiving cap will further strain families already providing around-the-clock care.
“While the state’s intent is to prevent caregiver burnout, the reality is that parents never clock out,” she said. “These programs simply make that care sustainable.”
But now she worries Medicaid cuts could imperil those programs or her son’s ability to have access to them.

The discrepancy had apparently been going on for years, after an error in billing code guidance given by the Department of Health Care Policy and Financing (HCPF) to the companies providing the services, according to a JBC analyst.
“We are taking this very seriously and are demanding that HCPF ensure it never happens again,” said Shelby Wieman, a spokesperson for Governor Jared Polis. “The agency is looking closely at irregular billing, and if found, would be investigated and prosecuted to the fullest extent of the law. We are taking actions like requesting future audits for the agency, and are working to ensure full transparency.”
For months, parents and advocates from a variety of groups have warned of dire impacts from proposed and potential budget cuts to the state’s Medicaid program, after Congress passed slashed funding for Medicaid last year.
Others representing families were sharply critical of the state agency that administers the state’s Medicaid program, called Health First Colorado.
"This is yet another instance of HCPF's incompetence. Regrettably, the people who suffer are the patients and families relying on Colorado Medicaid,” said Will Martin, co-chair of the public policy committee with the Colorado Association for Behavioral Analysis. “Instead of improving their processes and supporting providers, HCPF uses these situations to rationalize cuts to critical, life-saving services.”

He said the group has repeatedly warned HCPF about the inadequacy of their processes and standards, but those concerns were consistently disregarded. “Ultimately, children and families continue to suffer the most from HCPF's mismanagement."
Another advocate, Maureen Welch, the founder of Navigating Disabilities Colorado, a private LLC, echoed those concerns.
“It's terrible that this happened, but it kind of highlights the mismanagement and incompetence at HCPF,” said Welch, who has an autistic 18-year-old son. “Like to have a Medicaid HCPF employee tell them how to bill, and then it be wrong. That's just so demonstrative about so many issues in Medicaid.”
She said the transportation services for bariatric patients are important and should be properly funded. But she said as a result of these mistakes, legislators will have to find places to save that money elsewhere.
“But they're still not asking why (executive director) Kim Bimestefer is still in her position,” Welch said. “When someone doesn't do their job, they leave,” she added, noting that Cherry Creek School District superintendent Christopher Smith announced his retirement on Wednesday, following an investigation into allegations of a "toxic culture" within the district administration.
“Look at Superintendent Smith, the Cherry Creek school board finally pushed him out yesterday. We need the same at the state level. New management. New leadership.”
Others stopped short of that, but said they were surprised to learn of the overbilling errors.
“It's concerning that in yet another budget year where we're talking about really significant cuts, potentially to Medicaid, that we're finding an instance of spending that was not really warranted,” said Adam Fox, deputy director of the Colorado Consumer Health Initiative. “I think it is concerning that these providers have been receiving far above what would be expected, and we're gonna have to have conversations this legislative session about cuts to benefits and access for Coloradans.”
“The timing sort of couldn't be worse to find out mistakes like this because of the budget situation,” Fox said.
Gov. Jared Polis’ budget director answered questions about the billing mistake at a hearing before the legislature’s joint budget committee at the Capitol on Thursday.
In a text message to CPR News after the hearing, Mark Ferrandino, the head of the Office of State Planning and Budgeting, said the billing mistake doesn’t change the trajectory of increased Medicaid costs, and the fact that they are the biggest contributor to the state’s $800 million budget shortfall
“We are always looking to improve and identify issues, which much of our requests work on,” said Ferrandino. “But that work will not be enough to bend the cost trend and we need to make the hard decisions of how we bring the growth in costs to a more manageable level to ensure we protect coverage for the 1.2 million Coloradans who rely on Medicaid.”
Colorado has pointed to more people using Medicaid services, increased costs for medical care and expanded services as the primary factors for the higher price tag.









